TIM-3 Therapy for Alzheimer’s: A Promising New Approach
TIM-3 therapy for Alzheimer’s is emerging as a promising frontier in the search for effective Alzheimer’s disease treatment. Recent research suggests that targeting the TIM-3 checkpoint protein may enhance the immune system’s ability to combat the amyloid plaques that are hallmarks of this debilitating condition. By inhibiting TIM-3, scientists have observed improved plaque clearance by microglia—brain cells that play a crucial role in maintaining cognitive function. This innovative approach not only aims to restore memory in affected individuals but also brings a fresh perspective to how cancer therapies for Alzheimer’s might integrate with traditional treatment models. As researchers delve deeper into the relationship between the immune system and Alzheimer’s, the potential for effective interventions is becoming increasingly tangible.
The use of TIM-3 inhibition represents a novel strategy in combating Alzheimer’s, often interconnected with various immune responses and cognitive decline. In recent studies, the approach of deactivating TIM-3 has been linked to enhanced removal of harmful amyloid beta plaques, which build up in the brains of Alzheimer’s patients. By leveraging insights from cancer treatments, this method highlights a significant shift towards understanding the role of microglia in both plaque clearance and overall brain health. Consequently, this therapy could redefine approaches to Alzheimer’s, providing new avenues for exploring immune modulation in chronic neurodegeneration. The convergence of immune system insights with Alzheimer’s research presents an exciting opportunity to forge pathways that may revolutionize patient outcomes.
Understanding TIM-3 and Its Role in Alzheimer’s Disease
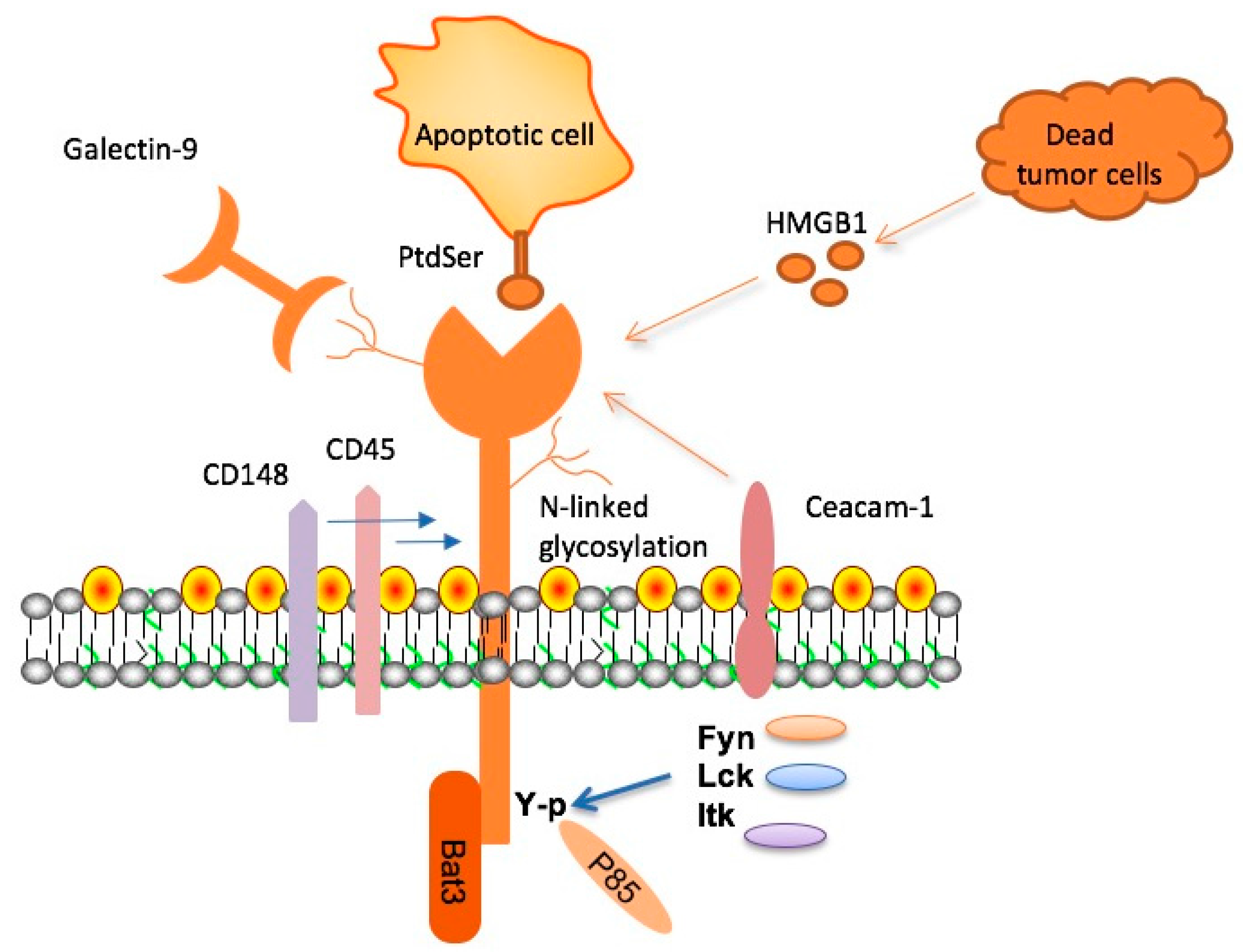
TIM-3, or T-cell immunoglobulin and mucin-domain containing-3, is an immune checkpoint molecule that plays a significant role in regulating the immune responses within the brain. Its primary function is to inhibit the activity of microglia, the brain’s resident immune cells. In the context of Alzheimer’s disease, the expression of TIM-3 is found to be significantly elevated in patients, particularly in association with amyloid beta plaques, which are hallmarks of the disease. This elevated expression poses a challenge, as it hampers the microglia’s ability to clear these toxic plaques effectively, leading to further cognitive decline.
Research has shown that the inhibition caused by TIM-3 prevents microglia from engaging in their phagocytic activity, which is essential for normal function and maintaining brain health. As we age, the accumulation of amyloid plaques is exacerbated, and the inability of microglia to act due to high TIM-3 levels contributes to the progression of Alzheimer’s pathology. By targeting TIM-3, therapeutic strategies may unlock the potential for microglia to resume their plaque-clearing functions, making it a crucial area of study for developing effective treatments for Alzheimer’s.
The Mechanisms Behind Microglia and Alzheimer’s
Microglia serve as the brain’s innate immune guardians, responsible for maintaining homeostasis, clearing debris, and supporting neuronal health. In healthy conditions, these cells actively prune unnecessary synapses, contributing positively to memory formation and cognitive function. However, their role becomes severely compromised in Alzheimer’s disease. The presence of amyloid beta plaques not only stimulates microglial activity but also leads to an aberrant state where TIM-3 becomes upregulated. This phenomenon prevents microglia from effectively responding to and clearing the accumulated plaques.
The accumulation of plaques results in chronic microglial activation, a condition characterized by an inability of these cells to perform their cleaning duties, ultimately leading to neuroinflammation. The negative feedback loop established by TIM-3 expression inhibits the necessary phagocytic functions and ensures that toxic buildups persist in the brain. Understanding this mutual reinforcement between amyloid plaques and TIM-3 expression is vital for developing potential interventions aimed at reactivating microglial functions, thereby restoring cognitive capabilities.
Advances in therapeutic approaches by targeting TIM-3 may pave the way for innovative Alzheimer’s disease treatments that focus on reviving microglial functions and enhancing the immune system’s ability to combat neurodegeneration.
Exploring Anti-TIM-3 Therapy for Alzheimer’s Disease
The emerging concept of anti-TIM-3 therapy for Alzheimer’s disease represents a promising frontier in neurotherapeutics. By utilizing monoclonal antibodies or small molecules that inhibit TIM-3’s function, researchers aim to bolster the microglia’s capacity to clear amyloid plaques. This approach could potentially alter the degenerative course of Alzheimer’s, making TIM-3 therapy an impactful strategy against this debilitating condition. It presents a creative blend of cancer immunotherapy principles and neurodegeneration treatment.
Early studies with TIM-3 depletion in animal models have already demonstrated improved cognitive outcomes and enhanced clearance of amyloid plaques. As researchers progress toward clinical trials, the primary focus will be on determining safe and effective dosages, as well as understanding how to facilitate this therapy’s delivery to the brain, given existing challenges with blood-brain barrier accessibility. The therapeutic implications of anti-TIM-3 antibodies could not only restore microglial functionality but also offer new hope for patients suffering from Alzheimer’s disease.
Linking Cancer Immunotherapy Concepts with Alzheimer’s Treatment
The parallels between cancer immunotherapy and Alzheimer’s disease treatment are becoming increasingly clear, particularly with agents targeting immune checkpoint molecules like TIM-3. Cancer therapies often involve unleashing the immune system’s ability to identify and destroy malignant cells by inhibiting checkpoints that otherwise restrain immune responses. Similarly, in Alzheimer’s, disabling TIM-3 could enable the brain’s immune cells, such as microglia, to target and eliminate damaging amyloid plaques that disrupt cognitive function.
Many recent breakthroughs in cancer treatment have started to incorporate strategies that enhance the innate and adaptive immune responses. The exploration of TIM-3 blockade within the Alzheimer’s framework aligns with these advancements, thus providing a novel angle that bridges both fields. Investigating immune system dynamics in the context of Alzheimer’s not only diversifies potential therapeutic approaches but also empowers researchers to explore multifunctional strategies that address the complexities of neurodegeneration.
Implications of Timely Intervention in Alzheimer’s Disease
The findings surrounding TIM-3 and microglia fundamentally reshape our approach to Alzheimer’s disease treatment, suggesting that timely intervention may have regenerative effects on cognitive abilities. Introducing anti-TIM-3 therapies could significantly alter the disease’s trajectory by enhancing the immune system’s role in plaque clearance. As clinical trials progress, the opportunity to demonstrate the benefits of such interventions serves as a beacon of hope for affected individuals and families.
Additionally, the integration of immune modulation strategies could lead to a more personalized approach to Alzheimer’s treatment. As researchers gain insights into patient-specific genetic factors, such as TIM-3 polymorphisms, therapies could be tailored to improve outcomes. This patient-centric view is essential as it may direct future Alzheimer’s research toward understanding individual variances in response to immunotherapies, leading to more successful treatment paradigms.
Combining TIM-3 Inhibition with Existing Alzheimer’s Therapies
Integrating TIM-3 inhibition with existing Alzheimer’s therapeutic models offers an innovative strategy for enhancing efficacy and improving patient outcomes. Current treatments targeting amyloid beta or tau proteins have shown limited success, driving the need for complementary therapies that could reposition or magnify their effects. By mitigating the inhibitory effects of TIM-3 on microglia, patients may experience enhanced plaque clearance alongside traditional approaches, addressing the multifaceted nature of Alzheimer’s disease.
This combined approach necessitates rigorous preclinical testing to assess the interaction between TIM-3 inhibitors and other Alzheimer’s therapies. The potential addition of immuno-modulatory components may also open pathways for combination treatment protocols that harness the overall capabilities of the immune system. As these research avenues unfold, the prospect of creating a viable multi-faceted treatment plan could set the stage for groundbreaking advancements in combating Alzheimer’s disease.
The Future of Alzheimer’s Research with TIM-3 as a Key Target
Looking ahead, the future landscape of Alzheimer’s research may heavily pivot around TIM-3 as a critical target. The advances from preclinical studies indicate that addressing TIM-3’s inhibitory role could not only enhance microglial functionality but may also hold implications for a broader understanding of neuroinflammatory mechanisms that underlie Alzheimer’s pathology. As scientific inquiry into TIM-3 evolves, predictive models of disease progression may incorporate the dynamics of immune checkpoints, helping to reshape diagnostic and therapeutic approaches comprehensively.
Furthermore, researchers’ focus on TIM-3 might spur innovative investigative avenues that converge upon the immune system’s role in neurodegeneration. By advancing our fundamental understanding of microglia’s interactions with amyloid beta and employing sophisticated genetic and molecular techniques, scientists can unlock valuable insights into the relationship between neuroinflammation and Alzheimer’s. This holistic view could lead to the identification of additional therapeutic targets, crafting a multi-target approach to tackling Alzheimer’s disease effectively.
Ethical Considerations and Challenges of TIM-3 Targeting in Humans
As promising as TIM-3 therapy for Alzheimer’s may seem, ethical considerations and inherent challenges in human trials demand careful scrutiny. The crossing of boundaries between cancer immunotherapy and neurodegeneration raises questions about the safety and efficacy of such interventions within vulnerable populations. Ensuring that any new treatment does not inadvertently trigger adverse immune responses or exacerbate existing neurological conditions will be paramount.
Additionally, the challenge of accurately assessing the long-term outcomes and potential side effects of anti-TIM-3 therapies necessitates robust monitoring protocols. Continuous evaluation of the balance between stimulating beneficial immune responses and avoiding adverse effects will be a central tenet of any related clinical programs. Maintaining transparency with participants about risks and benefits will also be crucial as healthcare providers seek to navigate this uncharted territory in Alzheimer’s research.
Conclusion: The Promise of TIM-3 in Alzheimer’s Disease Treatment
In conclusion, the exploration of TIM-3 therapy for Alzheimer’s disease represents a transformative potential within the realm of innovative treatments. By leveraging lessons learned from cancer immunotherapy, researchers are poised to redefine therapeutic avenues that target chronic inflammation and disrupted immune responses characterizing neurodegenerative diseases. The early signs of success in preclinical settings herald a new dawn for Alzheimer’s research.
As the understanding of TIM-3 continues to evolve, ongoing research must address the intricacies of the immune system in the brain and its relation to Alzheimer’s pathology. The prospects of restoring memory and cognitive functions through TIM-3 modulation stand to not only advance the scientific discourse but also foster renewed hope for millions affected by this relentless disease.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s and how does it work?
TIM-3 therapy for Alzheimer’s involves targeting the TIM-3 checkpoint molecule that inhibits microglial cells from clearing amyloid plaques in the brain. By blocking TIM-3, researchers aim to activate microglia to attack and remove these plaques, potentially improving cognitive function in patients with Alzheimer’s disease.
How does TIM-3 therapy relate to the immune system and Alzheimer’s disease?
TIM-3 therapy highlights the connection between the immune system and Alzheimer’s disease by focusing on how TIM-3 regulates microglial activity. Normally, TIM-3 prevents microglia from becoming overly active, which can hinder plaque clearance. By inhibiting TIM-3, researchers hope to enhance immune response against amyloid plaques, a hallmark of Alzheimer’s.
Can cancer therapies for Alzheimer’s utilize TIM-3 inhibition?
Yes, cancer therapies that involve TIM-3 inhibition are being repurposed for Alzheimer’s treatment. Since TIM-3 is targeted in cancer to boost immune response, similar strategies may help in Alzheimer’s by enabling microglia to effectively clear amyloid plaques, thereby improving memory and cognitive functions.
What role do microglia play in TIM-3 therapy for Alzheimer’s?
Microglia are the brain’s immune cells that typically help clear amyloid plaques associated with Alzheimer’s disease. TIM-3 therapy aims to enhance microglial function by inhibiting the TIM-3 checkpoint, allowing these cells to proactively eliminate plaques that contribute to cognitive decline.
Is TIM-3 therapy a potential breakthrough for plaque clearance in Alzheimer’s disease?
TIM-3 therapy represents a promising breakthrough for plaque clearance in Alzheimer’s disease. By blocking the TIM-3 checkpoint molecule, this therapy could restore microglial activity, enhance the removal of amyloid plaques, and potentially improve memory function in Alzheimer’s patients.
What is the significance of TIM-3 expression in patients with Alzheimer’s disease?
In Alzheimer’s disease, patients often exhibit elevated TIM-3 expression on microglial cells, which prevents effective plaque clearance. Understanding this expression profile is crucial, as inhibiting TIM-3 could rejuvenate microglial function and assist in combating the progression of Alzheimer’s.
How does TIM-3 therapy impact memory improvement in animal models of Alzheimer’s?
In animal models, TIM-3 therapy has been shown to improve memory by enhancing the ability of microglia to clear amyloid plaques. Mice that underwent TIM-3 inhibition demonstrated better cognitive performance in memory tasks, suggesting that similar strategies could benefit humans with Alzheimer’s.
What future research is planned for TIM-3 therapy in Alzheimer’s treatment?
Future research on TIM-3 therapy for Alzheimer’s includes testing human anti-TIM-3 antibodies in mouse models specifically designed to study Alzheimer’s. This will help determine the efficacy of TIM-3 inhibition in reducing plaque formation and improving cognitive deficits in humans.
What are the potential side effects of TIM-3 therapy for Alzheimer’s?
While TIM-3 therapy is designed to enhance plaque clearance, potential side effects may arise from altering immune response. Careful monitoring will be needed to ensure that boosting microglial activity does not lead to excessive inflammation or other adverse effects in the brain.
How effective is TIM-3 therapy compared to traditional Alzheimer’s treatments?
TIM-3 therapy could offer a novel approach compared to traditional Alzheimer’s treatments by directly enhancing the brain’s immune response to plaques. This strategy aims to address underlying causes of cognitive decline, potentially leading to more effective outcomes than therapies that primarily target symptoms.
| Key Point | Details |
|---|---|
| TIM-3’s Role in Alzheimer’s | TIM-3 is an inhibitory molecule on microglia that prevents them from clearing amyloid plaques in the brain, leading to memory issues. |
| Impact of Deleting TIM-3 | When TIM-3 was deleted in mice, microglia were able to clear plaques more effectively, which improved cognitive function. |
| Biodiversity of Alzheimer’s | Most Alzheimer’s cases (90-95%) are late-onset and linked to genetic factors such as TIM-3 polymorphisms. |
| Potential Therapy Approach | TIM-3 therapy could involve using anti-TIM-3 antibodies or small molecules that block TIM-3 function to enhance microglial activity. |
Summary
TIM-3 therapy for Alzheimer’s presents a promising avenue for treatment by utilizing the understanding of immune system mechanisms shown in recent research. By focusing on inhibiting the TIM-3 molecule, scientists can enable microglia to effectively clear amyloid plaques in the brain, which is crucial for restoring cognitive functions in patients. This innovative approach opens up possibilities for significantly improving the quality of life for those affected by Alzheimer’s disease.
You may also like
Archives
Calendar
| M | T | W | T | F | S | S |
|---|---|---|---|---|---|---|
| 1 | ||||||
| 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| 9 | 10 | 11 | 12 | 13 | 14 | 15 |
| 16 | 17 | 18 | 19 | 20 | 21 | 22 |
| 23 | 24 | 25 | 26 | 27 | 28 | 29 |
| 30 | 31 | |||||